Contents
Human Papillomavirus

Human papillomavirus (HPV), the primary cause of cervical cancer, is also associated with the development of anal cancer. Relatively little is known about the epidemiology of anal HPV infection among healthy females and its relationship to cervical infection. We sought to characterize anal HPV infection in a cohort of adult women in Hawaii. Overall, 27% (372 of 1,378) of women were positive for anal HPV DNA at baseline compared with 29% (692 of 2,372) with cervical HPV DNA. Among women with paired anal and cervical samples, anal infection without accompanying cervical infection was observed in 14% (190 of 1,363). Concurrent anal and cervical HPV infections were observed in 13% (178 of 1,363) of women. Women with cervical HPV infection had a >3-fold increased risk of concurrent anal infection. Concurrent anal and cervical HPV infection was most prevalent among the youngest women and steadily decreased through age 50 years. By contrast, the prevalence of anal infection alone remained relatively steady in all age groups. Compared with cervical infections, the overall distribution of HPV genotypes in the anus was more heterogeneous and included a greater proportion of no oncogenic types. A high degree of genotype-specific concordance was observed among concurrent anal and cervical infections, indicating a common source of infection. Nevertheless, the association of anal intercourse with anal HPV infection was limited to those women without accompanying cervical infection. The relationship of anal to cervical infection as described in this study has implications for the development of anal malignancies in women.
Introduction
Human papillomavirus (HPV), the primary cause of cervical cancer, is also associated with the development of anal cancers. A high prevalence of HPV infection in the anus has been observed in immunocompromised, HIV-infected men and women, but relatively little is known about the epidemiology of anal HPV infection among healthy women and its relationship to cervical infection. Although it is established that HPV infection can be transmitted to women through receptive anal intercourse, alternate routes of transmission may be possible.
As part of a longitudinal cohort study of cofactors of persistent HPV infection of the cervix, we sought to characterize contemporaneous HPV infection in anal specimens collected from cohort participants. Our objective was to determine the type-specific presence of anal HPV infection, with and without concurrent cervical infection, and to identify factors associated with anal-cervical HPV status.
Materials and Methods
In 1999, we initiated a multiethnic cohort in Hawaii to identify determinants of persistent HPV infection of the cervix. The study was approved by the Committee on Human Subjects of the University of Hawaii and individual hospital institutional review boards. Written informed consent was obtained from all study subjects. Eligible subjects included women ages 18 and older who were residents of Oahu. Women with a prior hysterectomy, who were pregnant within the past year, who had blood-clotting disorders, or who could not speak and understand English were ineligible to participate.
A total of 2,392 ethnically diverse women were recruited from five clinic sites in Honolulu, HI, and followed with repeat visits at 4-month intervals. Study sites included an urban medical center-based clinic servicing a largely indigent population, two university-based health clinics, a health maintenance organization, and a hospital-based clinical research center.
Cancers Linked with HPV
HPV (human papillomavirus) is known to cause many types of cancer in adults, including cancers of the mouth and throat, cervix, vulva, vagina, penis, and anus. More than 37,000 people get HPV-related cancers in the United States every year.
HPV vaccines can prevent more than 90% of HPV cancers when given at the recommended ages. Learn more about vaccination recommendations in HPV vaccines and about testing options in HPV testing.
Cervical cancer
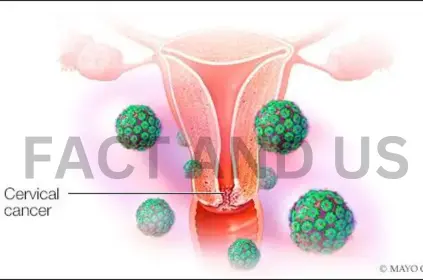
Cervical cancer is the most common cancer linked to HPV in people with a cervix. In fact, nearly
All cervical cancers are caused by HPV. Cervical cancer is preventable with the HPV vaccine
and regular screening tests.
Cervical cancer can be found early and even prevented with routine screening tests. Screening tests that are used include the HPV test and Pap test. The HPV test looks for an HPV infection. The Pap test looks for changes in cervical cells caused by HPV infection.
Vulvar cancer
HPV can cause cancer of the vulva. The vulva is the outer part of the female genital organs. This cancer is much less common than cervical cancer.
There’s no standard screening test for cancer of the vulva. Vulvar cancer might be found because a person notices changes or problems in their vulvar area or because a health care professional sees signs during a routine physical exam.
Vaginal cancer

Most cancers of the vagina contain HPV.
Many vaginal pre-cancers also contain HPV, and these changes may be present for years before turning into cancer. These pre-cancers can sometimes be found with the same screening test that is used to test for cervical cancer and pre-cancers. If a vaginal pre-cancer is found, it can be treated to stop further cell changes that can lead to cancer.
Penile cancer
HPV can cause cancer of the penis. Penile cancer is more common in men with HIV and those who have had sex with other men.
There’s no standard screening test to find early signs of penile cancer. Because most penile cancers start on the skin of the penis, they may be noticed early.
Anal cancer
HPV can cause cancer of the anus in both men and women. Anal cancer is more common in people with HIV and in men who have sex with other men.
Screening tests for anal cancer are not recommended routinely for everyone. Some experts recommend anal cytology testing (also called an anal Pap test) for people at higher risk of anal cancer. This includes men who have had sex with men, people who have had cervical cancer or vulvar cancer, or anyone who may have a compromised immune system (i.e., HIV-positive, anyone who has had an organ transplant).
Mouth and throat cancer
HPV is found in many oral (mouth) and throat cancers. Most cancers found in the part of the throat behind the mouth are HPV-related. These are the most common HPV-related cancers in men.
There’s no standard screening test to find these cancers early. Still, some can be found early during routine exams by a dentist, doctor, or dental hygienist, or by doing self-checks.
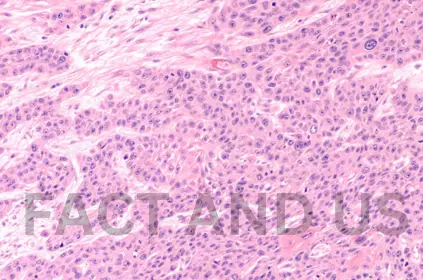
HPV DNA Testing and Genotyping
DNA was extracted from anal and cervical specimens using commercial reagents (Qiagen, Inc., Valencia, CA). The PCR reaction used a modified version of the original degenerate primer system, the PGMY09 and PGMY11 primer pairs with HMB01, which together amplify a 450-bp region of the L1 HPV genome. GH20 and PC04 primers were used to coamplify a 268-bp region of the human globin gene as an internal control for sample sufficiency.
Each 50 L reaction consisted of 1 PCR II buffer (Perkin-Elmer, Norwalk, CT), 6 mmol/L MgCl2 (Perkin-Elmer), 200 mol/L each of dATP, dTTP, dGTP, and dCTP (Perkin-Elmer), 7.5 units Ampliated Gold (Perkin-Elmer), 50 pmol each of PGMY09 and PGMY11 (Sigma, St. Louis, MO), 10 pmol HMB01 (Sigma), 10 pmol each of GH20 and PC04 (Midland Certified Reagent Co., Midland, TX), sterile H2O, and 5 L specimen DNA. Positive controls consisted of constructed plasmid DNA containing the entire genome of cloned HPV-16 DNA. Negative controls were void of template. PCR was done in a 96-well format on a Perkin-Elmer 9600 as follows: 95 C for 9 minutes; 40 cycles of 95 C for 30 seconds, 55 C for 1 minute, and 72 C for 1 minute; 72 C for 5 minutes; and 4 C hold.
Statistical Analyses
Women providing and not providing anal specimens were compared by unconditional multiple logistic regression. Odds ratios (OR) and 95% confidence intervals (95% CI) were computed by exponentiating the coefficients and 95% CI for the individual variables. Age (continuous variable) and race/ethnicity (White, Japanese, Hawaiian, Filipino, and other) were included as covariates.
The associations of risk factors with HPV status were also evaluated by unconditional multiple logistic regression, including age and race/ethnicity as covariates. Evaluation of anal-cervical HPV status was made using women negative for both anal and cervical infection as the reference.
Stay connected with Fact and US for more such news.
